Low-Dose Total Body Irradiation for Systemic Treatment of Cancer
Dr. Jerry Cuttler provided a copy of an open letter signed by 23 members or affiliate members of SARI – Scientists for Accurate Radiation Information that describes important information about the use of a specific regimen of whole (or half) body low dose radiation as a treatment in the continuing battle against cancer.
The organization has given Atomic Insights permission to republish the useful and informative document.
An Open Letter to Advisory Bodies Regarding
Low-Dose Total Body Irradiation for Systemic Treatment of Cancer
May 30, 2014
Dear Colleagues,
Though adjuvant chemotherapy has been a standard of practice in the systemic treatment of many cancers, its adverse side effects are of considerable concern. The possible side effects include anemia, fatigue, gastro-intestinal dysfunction, hair loss, infection, memory changes, etc. (1). These side effects diminish drastically the quality of life including long-term reduced physical functioning and overall general health (2). In addition, chemotherapy is associated with a life-long reduced rate of employment (3). Hence it is very important to seek alternative approaches for systemic therapy which have less harmful side effects.
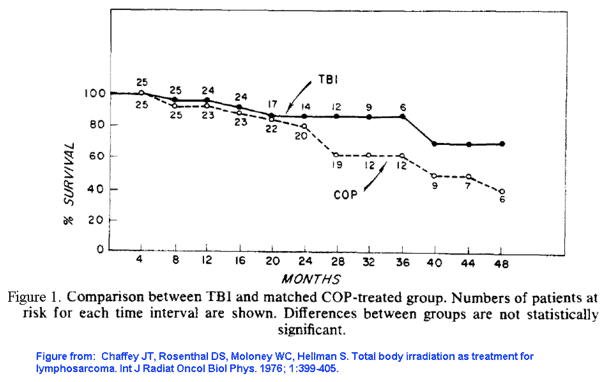
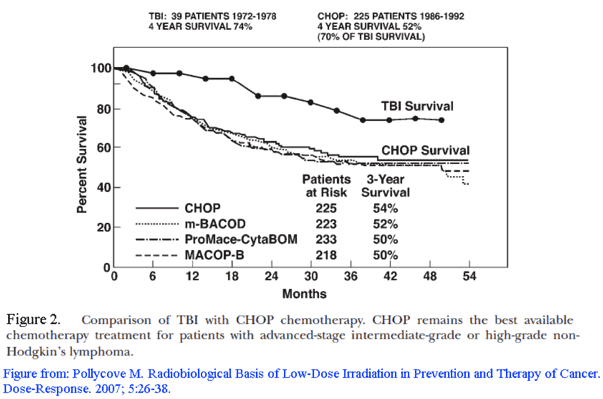
One adjuvant treatment that has similar or better outcomes with no symptomatic adverse side effects is low-dose fractionated total body irradiation (LDTBI). In the 1970s, LDTBI at the rate of 15 cGy per fraction, and 10 fractions applied over 5 weeks, had been studied in clinical trials of lymphosarcoma (4) and non-Hodgkin’s lymphoma patients (5). The 4-year survival rates with adjuvant LDTBI were equivalent (4) or better (6) when compared to adjuvant chemotherapy, as seen in Figures 1 and 2 below. The main short-term side effects from LDTBI were hematological, with no observed long-term adverse side effects (5).
One of the reported concerns regarding total-body irradiation (TBI) is the increased risk of leukemias when high-dose TBI was followed with chemotherapy (7). However, all the observed increased leukemias in this study were in patients who had high cumulative TBI doses of 2 Gy or more and/or high radiation doses to the bone marrow. LDTBI using a cumulative dose of 1.5 Gy has been studied clinically (8). The hematological side effects were temporary, minimal, and well-tolerated and the efficacy of the systemic treatment was significantly advantageous. Successful results in further clinical trials should lead to its widespread acceptance as a standard effective systemic treatment of cancers without the severe side effects of the current standard-of-care chemotherapies.
A major obstacle in initiating any clinical trial of LDTBI is the current use of the linear no-threshold (LNT) model for radiation risk assessment by regulatory agencies, based on recommendations of international and national advisory bodies. Because of the LNT model-based concerns, researchers may be reluctant to propose clinical trials of LDTBI. Thus, it is not surprising that LDTBI has been under-investigated and under-utilized in spite of its potential (9, 10). However, a considerable amount of evidence has accumulated clearly demonstrating that the LNT model is inconsistent with data (please see the compilation of evidence below).
In consideration of the above evidence, and in order to facilitate the study of this less deleterious systemic treatment of cancer, we ask you to make a declaration that you encourage the study of LDTBI for systemic cancer treatment, and that the LNT model, which is a conservative approach for calculating potential radiation risks, not be used to discourage the study of LDTBI.
We would be happy to discuss this matter with you or provide additional information for your consideration. Thank you for your kind attention to this important issue.
Sincerely,
Mohan Doss, Fox Chase Cancer Center, USA (mohan.doss@fccc.edu)
Allen Brodsky, Georgetown University, USA
Lu Cai, The University of Louisville, USA
Jerry Cuttler, Cuttler & Associates, Canada
Ludwik Dobrzynski, National Centre for Nuclear Research, Poland
Vincent J Esposito, University of Pittsburgh, USA
Ludwig E. Feinendegen, Heinrich-Heine University, Germany
Alan Fellman, Dade Moeller & Associates, Inc., USA
Krzysztof W. Fornalski, Polish Nuclear Society, Poland
Leo S. Gomez, Leo S. Gomez Consulting, USA
Marek K. Janiak, Military Institute of Hygiene and Epidemiology, Poland.
Brenda Laster, Ben Gurion University, Israel
Patricia Lewis, Free Enterprise Radon Health Mine, USA
Jeffrey Mahn, Sandia National Laboratories (Retired), USA
Mark L. Miller, Sandia National Laboratories, USA
Charles W. Pennington, Executive Nuclear Energy Consultant, USA
Jeffrey S. Philbin, Sandia National Laboratories (Retired), USA
Chary Rangacharyulu, University of Saskatchewan, Canada
Kanokporn Noy Rithidech, Stony Brook University, USA
Bobby R. Scott, Lovelace Respiratory Research Institute, USA (Retired)
Yehoshua Socol, Falcon Analytics, Israel
James S. Welsh, President-elect, American College of Radiation Oncology, USA
Ruth F. Weiner, Former Member of the NRC Advisory Committee on Nuclear Waste and
Materials, USA
Note: All signers of this letter are members or associate members of SARI (Scientists for Accurate Radiation Information, http://radiationeffects.org/). The above letter represents the professional opinions of the signers, and does not necessarily represent the views of their affiliated institutions.
References:
1. NCI. Chemotherapy Side Effects Sheets. [cited 2014 May 6,]; Available from: http://www.cancer.gov/cancertopics/coping/physicaleffects/chemo-side-effects.
2. Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002; 94:39-49. Available at: http://www.ncbi.nlm.nih.gov/pubmed/11773281
3. Jagsi R, Hawley ST, Abrahamse P, Li Y, Janz NK, Griggs JJ, et al. Impact of adjuvant chemotherapy on long-term employment of survivors of early-stage breast cancer. Cancer. 2014. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24777606
4. Chaffey JT, Rosenthal DS, Moloney WC, Hellman S. Total body irradiation as treatment for lymphosarcoma. Int J Radiat Oncol Biol Phys. 1976; 1:399-405. Available at: http://www.ncbi.nlm.nih.gov/pubmed/823140
5. Choi NC, Timothy AR, Kaufman SD, Carey RW, Aisenberg AC. Low dose fractionated whole body irradiation in the treatment of advanced non-Hodgkin’s lymphoma. Cancer. 1979; 43:1636-42. Available at: http://www.ncbi.nlm.nih.gov/pubmed/582159
6. Pollycove M. Radiobiological basis of low-dose irradiation in prevention and therapy of cancer. Dose Response. 2007; 5:26-38. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18648556
7. Travis LB, Weeks J, Curtis RE, Chaffey JT, Stovall M, Banks PM, et al. Leukemia following low-dose total body irradiation and chemotherapy for non-Hodgkin’s lymphoma. J Clin Oncol. 1996; 14:565-71. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8636772
8. Sakamoto K. Radiobiological basis for cancer therapy by total or half-body irradiation. Nonlinearity Biol Toxicol Med. 2004; 2:293-316. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19330149
9. Safwat A. The role of low-dose total body irradiation in treatment of non-Hodgkin’s lymphoma: a new look at an old method. Radiother Oncol. 2000; 56:1-8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10869748
10. Welsh JS. Waldenstrom’s Macroglobulinemia treated with fractionated low-dose total body irradiation. American Journal of Case Reports. 2004; 5:425-31. Available at: http://www.amjcaserep.com/abstract/index/idArt/12357
Note: The above Open Letter, including the compilation of ” Evidence for Threshold Dose-Response or for Radiation Hormesis in Human Studies” below, was e-mailed to the advisory bodies ICRP, NCRP, UNSCEAR, IAEA, WHO, and NAS on May 30, 2014.
After receiving the above letter, I made a special request to Dr. Cuttler. A couple of years ago, he told me a story that reinforced my understanding of his commitment to his research on the effects of low dose radiation and also demonstrated his high level of personal integrity.
You see, Dr. Cuttler not only talks the talk, but he walks the walk and advocates careful application of his research results to even his closest friends and family, including his wife, Vera. I asked if he and his wife would be willing to share their story about their own experience with low dose irradiation. He provided the following email.
From: Dr. Jerry Cuttler.
To: Rod Adams
Subj: Vera’s HB LDI treatment as prophylaxis
Vera agreed to share her story on Atomic Insights.
(This cost me my comfortable armchair, which will not move with us next month. She thinks the chair is ugly.)
Persistent bleeding after Vera’s annual PAP test, early in 2011, led to the discovery of a 1 inch tumor in her uterus. It was grade 3 (growing quickly), but at stage 1 (contained). After surgery in May, I asked about additional treatment to eliminate potential metastases. The radiation oncologist in Hamilton said this was unnecessary as a recurrence was unlikely. The options for follow-up treatment were chemo or high-dose irradiation in the abdomen, which would cause scarring. I asked about half-body low-dose irradiation (HB LDI) treatment. The oncologist hadn’t heard about this; she said it was not an accepted treatment. I asked for a referral to the cancer center in Mississauga, and I contacted Dr. Sakamoto. I described the case, and he recommended HB LDI treatment. He sent me an e-mail message that prescribed 15 cGy, twice a week for 5 weeks, a total of 150 cGy (150 rad). The hospital reviewed the case and agreed to provide this treatment because of the potential health benefit and the very low risk.
I first met Dr. Kiyohiko Sakamoto in June 1998 at an international symposium in Ottawa on health effects of low doses of ionizing radiation. He return in November 1999 for a meeting of the directors of the International Centre for Low Dose Radiation Research at the University of Ottawa (see attached photo). Dr Sakamoto later gave presentations at the Princess Margaret Hospital, at AECL (Mississauga) and at the Canadian Nuclear Society, Toronto Branch, along with Dr. Maurice Tubiana and Dr. Myron Pollycove. After the 2002 ASCO annual meeting in the USA, Dr. Sakamoto visited our home and met the family during our Thanksgiving Holiday dinner. And after participating in the International Symposium on Radiation Hormesis in Yokohama and Tokyo in November 2007, Vera and I visited Dr. Sakamoto and his lovely wife Keiko in their home in Sendai. We toured the lovely coastal area together, visiting charming villages and tourist attractions. Because of her familiarity with this subject, it didn’t take very much persuasion on my part to help Vera overcome her fear of this radiation treatment that Dr. Sakamoto had prescribed. The local radiation oncologist kept saying the risk is small, and I kept saying the benefit is very important.
HB LDI treatment was started in September. I asked that her blood variables be measuring periodically to collect data on its effect on her hemopoietic system. A blood sample was taken each week, just before the irradiation treatment. Vera was very apprehensive before the first treatment and was surprised by its short duration and the lack of any symptomatic side effects. She became less and less concerned at each visit. She said, “It’s nothing!” After each treatment, we went for breakfast and talked about any and everything. She told her worried girl friends all about her positive experiences. The only unpleasant part was the weekly blood samples. Their analysis showed no significant adverse changes to her blood cell concentrations. The depression in her platelet count was expected and temporary. However, the oncologist was very impressed to see the large boost in her immune system (NK cell) activity.
Jerry
Jerry Cuttler had many good reasons for recommending LDI therapy to his wife. He has been researching the topic professionally for more than a decade; one of the peer-reviewed papers he has published on the topic appeared in 2000 in the Canadian Nuclear Society Bulletin under the title of Application of Low Doses of Radiation for Curing Cancer.
One more personal note: One of my very best friends and former workout partners was diagnosed with ovarian cancer about ten years ago at age 35. She had surgery, chemotherapy and high-dose irradiation in the abdomen. The doctors informed her before conducting the treatment that she would never be able to have children. After a very difficult recovery from the painful, scar-causing treatment, she lived well for several years. Eventually, she had a recurrence that proved fatal.
Though I have no medical training, it seems so logical to think that a low dose regimen that worked to stimulate her immune system rather than destroying it would have provided better results.

Cigarette, anyone? (Bottom of page 3)
http://legacy.library.ucsf.edu/documentStore/p/w/c/pwc42f00/Spwc42f00.pdf
Oh, to be unencumbered by logic…
https://yourlogicalfallacyis.com/genetic
This is a good story for it tells of scientific and results-based discussions. We need more Jerry Cutlers sending these positive and evidence-based messages. Well done Jerry.
Dear Vince
Thanks for your comment. I’m delighted that you are so interested in these real life happenings. Yes, we need to hear additional positive messages.
Many people are spreading false scare stories that are so harmful.
Regards
By the way, the lovely coastal area near Sendai that Dr. Cuttler visited in 2007 happens to be the area that has been most completely destroyed by the tsunami, and has suffered the largest share of it’s human loss.
Did you note Figure One, the straight line data indicating a very low sample size, and the annotation, The differences are not statistically significant.
Actually, you don’t have to look hard for any “indication” of the sample size. The graph expressly notes that each group started with 25 people.
Some of us did note that, and it’s incredibly interesting. Just because the difference isn’t statistically significant and the sample size is small doesn’t mean that it doesn’t say lots. The first thing that I draw from it is that high doses of radiation aren’t that bad. 1.5 Gy in 5 weeks is a lot of radiation, and if you listen to many people this should have many serious health effects but this was not observed. The second thing is that LDTBI worked as well as COP, if not better, with fewer side effects. I’d call that a win, but cancer treatments have improved dramatically since the 1970’s so I’m not sure how it would go now. We have also improved hugely since the early 1990’s in case you look at fig. 2. Given that LDTBI works via a different mechanism to (most) chemotherapy it is quite possible that both therapies could be used concurrently for enhanced effect. There is more than enough evidence to at least continue research in the field, particularly given that the risks of further research are low and the rewards are potentially huge.
@Australian Physicist
Exactly. The whole point of the open letter is summarized in the penultimate paragraph:
Rod, thanks for your excellent blog, a much needed antidote to anti-nuclear hysteria.
I think referring to the 1.5 Sievert dose of this systemic cancer treatment as “low dose” is not helpful. Yes, it is much lower than the dose in radiation therapy, but by any other standards it seems a whoppingly high dose. The message that needs to come across is that even at these doses, damaging side effects are to small to be observable. Which tells us a lot about the maximum likely harm from the orders of magnitude smaller doses members of the public or even emergency workers at Fukushima.
The 1.5 Sv is the sum of ten fractions of 0.15 Sv each.
Each low dose of 150 mSv up-regulates the adaptive protection systems (~200 genes) that and coping continuously with the endogenous DNA and other cell damage that is occurring at an enormous rate.
After several days of recovery, another 150 mGy dose can be delivered, and there are no symptomatic adverse side effects.
After six months, Dr. Sakamoto provided a “booster” of the same 1.5 Sv treatment to his cancer patients.
Dr. Cuttler,
Thank you for advancing medicine in the face of certain disparagement because you challenge firmly-entrenched beliefs.
Your work brings to mind the “Hygienic Hypothesis” and helminthic therapy. The very thought of intestinal parasites as therapy seems like quackery — until one looks at the results.